Information for mothers of newborns
With a 220-year history, the East Tallinn Central Hospital Women's Clinic has been recognised as a baby-friendly hospital since 2008.
This means that:
-
in our hospital, children are not separated from their mothers;
-
we encourage skin-to-skin contact between parents and babies, laying the foundation for successful breastfeeding;
-
we know that the unique living tissue called breast milk is the most valuable food for a newborn.
Good to know!
-
Stay awake while breastfeeding and monitor your baby’s well-being!
-
Always lift your baby with both hands and without rushing to prevent dangerous accidents!
-
Use a baby stroller when moving around the hospital with your baby.
Congratulations – you have become a parent! The purpose of this booklet is to provide information about the changes that occur in a woman's body after childbirth and recommendations on how to cope with them. It also includes information on how to successfully breastfeed your baby and practical tips on managing life at home with a newborn.
SAFETY AT HOME
To ensure a safe environment for your baby and to avoid accidents, parents can assess their home early on and take measures to increase the safety of their baby and prevent accidents.
Your baby's wellbeing depends 100% on adult care.
Safe sleep:
1) Always place your baby to sleep on their back. Do not let infants sleep on their stomach until they have learned to roll over on their own.
2) The child should sleep in their own crib, cradle or stroller. Do not sleep in the same bed as your baby. If you want the baby to sleep close to you, place the crib near your bed.
3) The baby’s crib should have a firm mattress and a flat surface. The child should never sleep on a soft sofa, a bed or other soft surfaces. It is also not advisable to let your child sleep on an air mattress. Never let your child sleep in a car seat, except when in the car.
4) Keep all pillows, soft toys and other soft items out of the baby’s crib. Do not use crib bumpers.
5) Do not cover the baby's head during sleep.
6) Dress the baby in layers to keep them warm without overheating. You can also try a sleeping bag according to your baby’s size and weight. Avoid using weighted blankets or swaddle blankets.
7) Keep the room temperature at a reasonable level to avoid overheating the child.
8) Quit smoking and do not allow anyone to smoke in your home or car.
9) Breastfeed your baby, if possible.

A safe sleep environment for 0-1 year olds
BREASTFEEDING
Breastfeeding is the best and simplest way to feed your baby during their first year of life. The World Health Organization recommends exclusively breastfeeding for the first six months and continuing breastfeeding into the second year of life if possible.
Breast milk and its production is a natural phenomenon. After birth, hormonal changes in the body trigger milk production. Depending on your baby's nursing dynamics, the amount of milk increases and its composition changes between the second and fourth day after delivery.
Colostrum is the first milk produced in the breasts and is already present during pregnancy and the first days after birth. The amount of colostrum is not great. It is excreted in small drops and contains everything your baby needs in the first days of life – nutrients, vitamins and antibodies.
In addition, colostrum:
- protects the baby from infections;
- reduces the likelihood of developing non-communicable diseases;
- prepares the baby's immature digestive system for digestion;
- protects the baby from jaundice due to its laxative effect.
From the second day of life, the baby should be offered the breast as often as they demand and at least eight times a day. The interval between feedings during the day should not exceed three hours and the baby should be woken if necessary.
Frequent breastfeeding stimulates milk production and increases the fat content of the milk.
The baby should not be offered a bottle or a pacifier in the first month of life as these may prevent the baby from learning how to latch on correctly.
In the first six months of life, your baby gets everything needed for growth and development from breast milk. No extra fluids (water, tea, juice) are needed during this time.
Your baby is getting enough breast milk if:
- they eat at least eight times a day;
- they urinate frequently, at least six to eight times a day;
- after two weeks, their stool has become yellow and has a sour smell; sometimes the poo can be runny. The frequency of bowel movements varies greatly among breastfed babies. It is perfectly normal for a baby to poop after each feeding or only once a week;
- they gain at least 500-600 grams per month (the first month’s weight gain should be calculated from the lowest known weight, not the birth weight);
- they grow in length.
Your baby does not get the same amount of milk with each meal and their day/night rhythm has not yet developed. Some babies may nurse for a long time – 30 to 40 minutes at a time and then rest for an hour. Others want to nurse for shorter periods but more frequently and some feed quickly and are satisfied with three-hour intervals. We recommend offering both breasts during each feeding session. If the baby is positioned correctly, they can nurse for as long as they want, but we suggest limiting nursing sessions to 40 minutes to ensure adequate rest between feedings.
Over time, your baby will develop their own feeding pattern, but it is still important to ensure that they are fed at least eight times a day.
Once you are producing enough breast milk, we recommend helping the baby burp after each feeding session by holding them upright (for up to 10 minutes) either in your arms, against your chest or over your shoulder. Sometimes babies burp very audibly and quickly in an upright position, other times the ‘burp’ may occur just before the next feeding.
It is not recommended to perform major care activities (such as changing diapers or clothes) immediately after feeding as this can cause the baby to spit up excessively. If changing is necessary, do it carefully, making sure not to lift your baby’s legs too much or press strongly on their belly or turn them from side to side too abruptly.
Signs of a good latch (Figure 1):
- The baby's whole body is turned towards the mother – they are pressed against each other belly to belly.
- Before attaching to the breast, the baby's nose is aligned with the mother's nipple.
- The baby’s mouth is wide open, head slightly tilted back, with a double chin.
- The baby’s nose, chin and cheeks are pressed against the mother's breast.
- The baby's bottom lip is turned outwards.
- The baby’s cheeks are round and there are no dimples during sucking.
- Sucking alternates with swallowing.
- After breastfeeding, the nipple is rounded, not triangular; the breast feels softer.
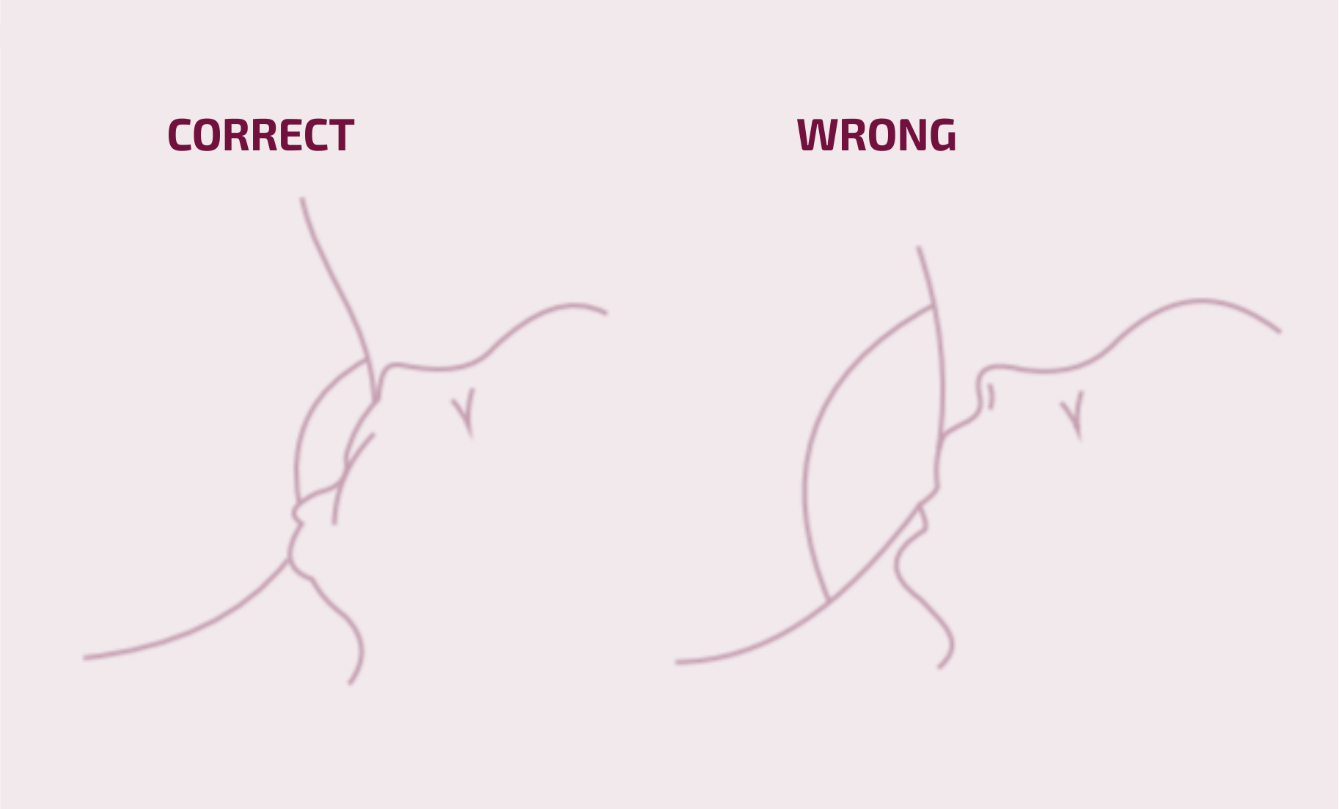
Figure 1. Author Ülle Lember (from the Estonian Birth and Breastfeeding Support Society (SIET) leaflet ‘Breast Milk is Best for Your Baby’, Part II)
Remember!
- Wash your hands before breastfeeding!
- The breast is always clean and does not need preparation.
- Choose a comfortable position for breastfeeding as a newborn may take longer to feed.
Breast engorgement and sore nipples
Breast engorgement most commonly occurs between the second and fifth day after delivery when the amount of milk in the breast increases significantly. The breasts may become heavy, hot, tender and hard. You may develop a low-grade fever (up to 37.5 °C) that usually subsides on its own if you breastfeed frequently. Engorgement tends to be less severe if the baby is breastfed frequently from the early days. The symptoms usually resolve in around seven days.
How to relieve engorgement symptoms
- Your baby should be breastfed frequently.
- Ensure that your baby has the correct latch.
- During feeding breaks, apply a cold, clean cabbage leaf to the breast. Change it every four hours or more often.
- Before feeding, express a small amount of milk from the breast to reduce swelling and make it easier for your baby to latch. This is often more successful in a warm shower or using a warm compress.
- If the breasts remain sore and hard even after breastfeeding, apply something cold to the breast for 15 to 20 minutes after feeding.
In the first few weeks after giving birth, your nipples may be sensitive or sore, even if the baby is latching on properly. In this case, apply a lanolin-containing soothing ointment to the nipples after feeding.
Nipple cracks indicate an incorrect latch. Carefully monitor your baby's latch.
How to increase milk supply
The more frequently your baby nurses, the quicker your body will learn to produce the necessary amount of milk. Breastfeeding is more successful if you give yourself and your baby time to learn.
Rest with your baby. While still in the hospital, learn how to breastfeed while lying down. Lying down with your baby makes it easier to get used to breastfeeding both at night and during the day. Breastfeeding at night increases milk production.
Follow a balanced and nutritious diet. The composition of breast milk is not directly dependent on the mother's diet, but eating and drinking regularly and nutritiously is important for your well-being. The best thirst quencher is water.
Hand expressing breast milk
Hand expression is a technique used to remove milk from the breasts using your fingers.
Hand expression is an important skill for:
- reducing engorgement symptoms;
- stimulating and maintaining lactation if the baby is unable to nurse effectively;
- increasing the amount of milk in the breasts.
How to hand express breast milk
- First, wash your hands thoroughly and choose a clean container to express the milk into.
- Get into a comfortable position.
- Before expressing, it is recommended to have a warm drink, apply something warm to the breast, gently massage the breast and stroke the breast towards the nipple to help milk flow better.
- To hand express, place your thumb and index finger about 3 cm away from the nipple so that your hand forms a C-shape, with the nipple positioned in the middle of a straight line between your fingers (Figure 2).


Figure 2. Position of fingers when expressing breast milk by hand.
- Compress the breast between your fingers towards your chest, rhythmically press the nipple several times and collect milk droplets into a container (Figure 3).


Figure 3. Manual expression of breast milk.
It may take a few minutes for the milk to flow, so be patient. After a while, change the position of your fingers on the breast to empty other milk ducts. Then move to the other breast and repeat the process.
STORAGE OF BREAST MILK
- Expressed milk must be stored in a clean and closed container.
- Label the container with the date and time of expression.
-
Storage Fresh breast milk (at room temperature) four hours In a standard refrigerator (4-8 °C) four days In a freezer six months Thawed breast milk 24 hours in the refrigerator - To feed the baby, the mother's breast milk can be stored at room temperature for four hours from the start of collection.
- Freshly collected (manually or with a pump) breast milk does not need to be warmed and can be used immediately at room temperature.
- The milk that needs to be stored should be placed as far away from the door in the refrigerator as possible so that the temperature fluctuations caused by opening the door do not affect the stored milk.
- Do not add freshly expressed warm milk to already chilled or frozen milk in the refrigerator. It is best to chill freshly expressed milk before adding it to previously collected and chilled milk.
- Breast milk that has been collected and chilled over the course of a day can be combined together in the same storage bag and placed in the freezer. BE SURE to mark the date!
- Frozen breast milk (-4 °C to -20 °C) lasts up to six months. Be aware that milk expands when frozen. Leave some space at the top of the storage container (plastic food storage bottle, freezer bag, etc.) as milk expands with freezing. All breast milk collection containers must be labelled with the date of collection and the name of the baby or mother. Store in small portions (e.g. 50, 60, 100, 120 mL) to avoid wasting the thawed breast milk later.
PREPARING BREAST MILK FOR USE
- Preferably use fresh breast milk (no older than four hours) for feeding as it is always of higher quality than chilled or frozen milk. Fresh milk contains antioxidants, vitamins, proteins, fats, probiotic bacteria and maternal secretory IgA antibodies and has the highest immunological activity.
- Options for thawing frozen milk
- Place the required amount of frozen breast milk in the refrigerator to thaw for 24 hours. Slowly thawed breast milk can be used the next calendar day.
- Frozen breast milk can be thawed in room-temperature water by placing the containers in a bowl of room-temperature water. However, slow thawing in the refrigerator is preferred, as this reduces fat loss compared to thawing in warm water.
- You can also thaw frozen breast milk by heating it without water, i.e. thawing it at room temperature.
Heating breast milk to body temperature
- Warm breast milk taken from the refrigerator to body temperature: this is easiest done with lukewarm water (maximum 40 °C) for 20 minutes. Pour the milk into a container (with a screw cap or a syringe) and place it in lukewarm water, i.e. a water bath, to warm it up (e.g. for breastfeeding).
- If hot water (>40 °C) is used, the time in the water bath will be shorter. PLEASE NOTE! ALWAYS check the temperature of the warmed milk on your wrist by dripping a few drops on your skin. If the temperature of the warmed breast milk is suitable, mix it before giving it to your baby.
- Rapid warming of breast milk (with boiling water or in a microwave) is not allowed as it does not allow the milk to mix properly. The milk heats unevenly, resulting in a reduction in the fat content and the activity of bioactive substances.
Using and refreezing thawed milk
- Do not refreeze thawed breast milk!
- Discard any excess thawed breast milk.
Giving thawed milk to the baby
The milk should be at body temperature before giving it to your baby, but no hotter than 37 °C. Check the milk temperature on the back of your hand or with a liquid thermometer before giving it to your baby. Thawed breast milk should be used within two hours. Preferably, give the milk to your baby with a small cup, bottle or spoon.
Using colostrum collected before birth
Colostrum collected before birth should be stored in closed containers, such as 1-5 mL syringes with caps. Containers of colostrum must be labelled with the mother’s name and the date of collection. To take to the hospital, place the containers in a Minigrip plastic bag and maintain the cold chain during transport. Containers of colostrum stored in Minigrip bags are kept in the freezer section of the refrigerators designated for patients in the maternity ward. Pre-expressed colostrum may be needed in the first days of life for newborns at risk of hypoglycaemia or with developmental anomalies diagnosed during pregnancy that complicate breastfeeding.
All babies are different and therefore you may have questions about breastfeeding. Seek help before a question becomes a problem!
BREASTFEEDING COUNSELLING
It is recommended to visit the midwife-breastfeeding counsellor with the baby.
Breastfeeding counselling is free and available in Estonian, Russian and English.
To schedule an appointment or phone counselling, call +372 666 1900 on weekdays or register via terviseportaal.ee.
The breastfeeding counselling office provides help to mothers who have problems with breastfeeding or the health of their breasts. The breastfeeding counselling office can be contacted for any issues regarding breastfeeding – condition of the breasts, soreness, baby's sucking behaviour, weight gain questions, age-appropriate supplementary food, weaning, etc. Additional information is available at: https://www.sunnitusmaja.ee/sunnitus/sunnitusosakond/imetamisnoustamine/
Breastfeeding counselling offices:
Ravi unit (Ravi 18) on the first floor of the maternity hospital, Room 128.
- The office is open on weekdays.
- Phone counselling is available at +372 620 7453.
Järve unit (Energia 8) on the first floor, Room 118.
- The office is open on weekdays.
- Phone counselling is available at +372 606 7606.
Magdaleena unit (Pärnu mnt 104) on the first floor, Room 120.
- The office is open on weekdays.
- Phone counselling is available at +372 606 7849.
NEWBORN CARE
We recommend carrying out care routines during a diaper change before breastfeeding.
CHANGING AND DRESSING
You can wrap your baby freely, without wrapping their arms. Disposable diapers can be used, but keep the umbilical wound free (fold the diaper edge down). No hats or gloves are needed indoors.
Choose comfortable and skin-friendly clothing for your baby, avoiding long straps or cords that the baby might get tangled in. When dressing your baby, take into account the room or outside temperature. It is good to dress the baby in layers, which allows you to remove or add clothing as needed to prevent overheating or hypothermia. Body temperature regulation develops over the first year of life. The weak functioning of sweat glands increases the risk of overheating in high temperatures. Overheating is one of the causes of sudden infant death syndrome.
The changing mat should be intact, safe, have high edges and be slip-resistant. Have everything needed for swaddling, dressing or cleaning the baby within reach.
Do not leave your baby unattended on the changing mat.
UMBILICAL CORD AND UMBILICAL CARE
The umbilical cord stump dries and detaches within 3 to 45 days of life, most commonly between the 8th and 14th day.
For umbilical care, prefer a dry and open method.
A normal umbilical area is dry and not red. Clean the umbilical area with boiled (cooled) water. It is important to clean around the edges of the umbilical stump by gently pulling the umbilical cord stump outwards from the umbilical band or clamp. Moving the umbilical stump is not painful for the baby. This can be done a couple of times a day, also after bathing. Leave the umbilical area exposed and do not cover it with gauze or a plaster. After the stump falls off, the umbilical wound should be cleaned three to four times a day for about a week until it heals completely. If the umbilical area appears red, swollen, has an unpleasant smell or oozes, contact your family doctor.
BATHING
Your baby can be bathed on the same day after arriving home from the maternity hospital, except if the baby was vaccinated that day. The recommended bathroom temperature should be at least 25 °C, bath water should be 37 °C. Regular tap water is suitable for bathing; no additives are needed. You can bathe every day, but only use baby soap one to two times a week, otherwise the skin will dry out too much. The umbilical area may get wet during bathing. If possible, give the bath at the same time each day. If your baby’s skin is dry, you can apply a baby-friendly lotion or moisturising baby cream. After bathing, put a hat on your baby until their head is dry.
An evening bath usually brings a good night's sleep.
SKIN CARE
The best tool for newborn skin care is clean water. Use running tap water to clean the diaper area. Avoid using wet wipes. If problems develop (e.g. dry skin, chafing, rash or inflammation), use special baby skin care products. If your baby’s skin is dry, it can be moisturised several times a day. To prevent chafing, it is important to dry all folds thoroughly after washing, including behind the ears, the chin fold, the armpits and the groin area. If there is redness, inflammation or rash on the skin, consult a family doctor.
CLEANING THE EYES
The goal of eye care is to keep the eye area clean and support the opening of congenital tear duct obstructions through a massaging eye-cleaning technique. In most cases, congenital tear duct obstruction resolves spontaneously during the third week of life. Symptoms of a congenital tear duct obstruction may include watery eyes and discharge.
For more information: https://www.itk.ee/patsiendile/patsiendi-infomaterjalid/haigused/pisarateede-kaasasundinud-sulgus-imikutel
Clean the eyes from the outer corner towards the inner corner with warm boiled water, using a separate cotton ball for each eye. Preferably, use cosmetic wipes sold at pharmacies that do not shed lint.
Eye care should be performed at least twice a day, for example, in the morning and in the evening. More often if necessary
CLEANING THE NOSE
Newborns sometimes tend to ‘sniffle’. Your baby's nasal passages may be swollen due to dry air and the mother's hormones. In this case, you can use saline nasal drops to moisturise the mucous membranes and reduce swelling. Your baby may then sneeze, expelling softened crusts from the nasal passages. Remove these with a tissue. If there is a lot of secretion in the nose that disturbs your baby’s usual state, you can use a nasal aspirator.
NAIL CUTTING
It is best to cut your baby’s nails during sleep, when they are calm and not actively moving. Use baby nail scissors or clippers with rounded tips. Ensure that scissors with sharp tips have curved ends. Trim nails slightly and only the sharp edges to avoid scratching or injury. The nails are cut straight across to prevent ingrown nail corners. If you accidentally injure the surrounding skin, put a plaster on the injured area.
FIRST OUTDOOR WALK
You can start taking the newborn outside right after birth if you feel ready, the baby is healthy and the paediatrician has not advised against it.
Pay attention to extreme weather conditions. Do not leave your baby to sleep in direct sunlight as there is a risk of overheating. In cold winter weather, it is advisable to practice sleeping indoors with an open window for a few days. You can go outside when your baby is a week old, preferably not in weather colder than -10 °C.
Your baby is dressed appropriately when the area between the neck folds is warm after coming in from outside.
STOOL
The baby's stool is blackish green in the first few days. This type of faeces is called meconium. Over the next two weeks, the stools become yellow and sour-smelling, sometimes the stool may be liquid. The frequency of stool for a breastfed baby varies (from after each feeding to up to once a week)
GAS PAINS
As your baby’s digestive system adjusts to independent digestion over the first two to three months, gas pains may occur more frequently. There are no specific medications for this as the causes of excess gas are varied.
Some recommendations
- After feeding, hold your baby upright for a few to ten minutes to allow any swallowed air, or ‘burps’, to be released.
- Place your baby on their stomach for half an hour two to three times a day. It strengthens the abdominal muscles. Do not leave your baby unattended during this time.
- To relieve gas pains, gently rub the abdomen in a clockwise direction.
- Since gas pains are most common in the afternoon or evening, try to schedule baths during these times. Warm water helps relax and release gas more easily.
- Several over-the-counter medications for gas relief are available: Sab-Simplex and Espumisan. Consult your family doctor before using them.
BODY TEMPERATURE
After birth, the newborn's body temperature depends on the temperature of their environment. A child's normal body temperature is 36.5-37.3 °C. If the temperature of the surrounding environment is right for your baby, the baby will not sweat or be restless due to cold. The appropriate temperature may vary between babies and will change during the first weeks of life.
Hypothermia is a condition where the body temperature is below 35 °C. Premature and/or underweight newborns are more likely to be unable to maintain body temperature.
Hyperthermia, or overheating, is a condition where the skin temperature is above 38 °C. If not due to an illness, the most common cause of elevated temperature is an overly warm environment (breastfeeding, too many clothes, etc.).
VITAMIN D
From the 7th day of life, start giving your baby vitamin D. If your baby is exclusively breastfed, the amount of vitamin D is 400 active units (IU) once daily before feeding. We recommend continuing to give vitamin D also in the second year of life. If your baby eats at least a litre of formula a day, vitamin D is not needed. In the case of combined feeding, the doctor calculates the vitamin dosage. Vitamin D is available in pharmacies without a prescription.
TRAVELLING WITH A BABY IN A CAR AND IN TRAFFIC
Always use a crash-tested car seat appropriate for your baby’s weight category; replace it in a timely manner with a safety seat, as most are designed for use up to 15 months of age or according to weight category. Place the car seat only in a rear-facing position.
Your baby must not be in a car seat next to the driver if the front airbag is activated.
Your baby should lie at a 45-degree angle in the car seat; an overly upright position can cause the baby’s chin to fall to their chest, potentially causing breathing difficulties, to the point where the baby cannot breathe at all. It is recommended to take only short trips of up to two hours. Prolonged time in a car seat can strain the baby’s neck and back.
Do not leave your baby alone in the car, even for a short time.
POSTPARTUM SELF-CARE AND RECOVERY
The postpartum period begins with the delivery of the placenta and ends approximately six to eight weeks after childbirth. During this time, the hormonal and physiological changes that occurred during pregnancy and childbirth subside.
Postpartum discharge from the vagina lasts for six to eight weeks. This is due to the healing of the uterine lining. Dangerous bleeding can occur within 24 hours after birth, but significant bleeding may also occur during the first postpartum week, rarely later. If you experience bleeding, fever or foul-smelling discharge, seek emergency care at the women’s clinic.
After childbirth, use only sanitary pads and perform daily intimate hygiene. You can go to the bath, pool or sauna once the bleeding has stopped.
You may use a binder or support belt for abdominal support if desired. Do not cover the wound area with a binder after a caesarean section.
POSTPARTUM PERINEAL CARE
In the first few days after birth, there may be perineal swelling and tenderness due to tissue stretching and tearing. Stitches are absorbable and perineal swelling usually subsides within a couple of weeks.
- For severe perineal trauma, avoid sitting upright on your bottom for three to five days. Sit on a cushion with a hole in it or make your own U-shaped seat.
- After each toilet visit, wash the perineal area with clean running water from front to back to prevent infection.
- If possible, let the wound air-dry.
- For swelling, you can apply a cold compress to the wound.
- Once the pain and swelling subside, you can start training your pelvic floor muscles.
MENSTRUATION AND SEXUAL INTERCOURSE
If you are not breastfeeding, the first menstruation is typically expected four to eight weeks after delivery. Menstruation may be absent while breastfeeding, but usually resumes after breastfeeding is stopped.
Sexual activity can be resumed once bleeding has stopped and you feel ready. Breastfeeding does not protect against pregnancy. If you want to avoid pregnancy, use a condom. Other contraceptive methods will be discussed at the postpartum visit.
ABDOMINAL PAIN
Abdominal pain due to uterine contractions can occur for up to a few weeks after delivery. Painful uterine contractions are more common in women who have given birth before and during breastfeeding due to the release of the hormone oxytocin. The uterus will return to its pre-pregnancy size within a few weeks.
For pain relief, paracetamol 1000 mg three times a day or ibuprofen 400 mg three times a day can be used for a short period.
URINATION
After childbirth, there may be bladder overfilling or incomplete emptying. Go to the bathroom regularly every three hours. If urinating is difficult the first few times, using warm running water can help. Spontaneous urinary incontinence may occur in the first few postpartum months but usually resolves with pelvic floor muscle training within three to six months.
CONSTIPATION
To avoid constipation, drink plenty of fluids, at least one and a half litres per day. A well-balanced diet also helps with constipation. Use lactulose-containing laxatives, if necessary.
HAEMORRHOIDS
Haemorrhoids are enlarged veins in the anal area. There are external and internal haemorrhoids. Haemorrhoids may cause pain. For pain relief, you can apply an ice pack to the painful area or use over-the-counter medications designed for this purpose.
PELVIC FLOOR MUSCLE TRAINING
Relevant information can be found in the patient information leaflet: Postpartum and caesarean recovery https://www.itk.ee/patsiendile/patsiendi-infomaterjalid/enesehooldusest/proper-movement-patterns-and-muscle-training-for-postpartum-recovery
FOLLOWING A CAESAREAN SECTION
A caesarean section is an operation where the baby is born through an incision made in the abdominal wall and the uterus.
At home, you can take paracetamol 1000 mg three to four times a day and/or ibuprofen 400 mg three times a day as pain relief, unless otherwise directed by your doctor. The wound dressing will be removed 24 hours after surgery. Whether or not the stitches need to be removed will be decided by your doctor. The sooner you start moving around, the faster the recovery from surgery. At least once a day, shower and wash the wound with running water, soap or shower gel. Airing out the wound also helps speed up healing. After a caesarean section, you may experience pain in the shoulder or neck area. In such cases, use over-the-counter painkillers in the doses mentioned above. Avoid lifting heavy objects (>6 kg) for six weeks.
EMOTIONAL STATE AFTER CHILDBIRTH
Childbirth and the postpartum period are associated with various and often significant emotions.
Two-thirds of mothers experience baby blues or maternal sadness. A few days to a couple of weeks after birth, there may be emotional ups and downs, such as tearfulness, excessive anxiety or a feeling of emptiness.
The responsibility of having a baby can cause worrying thoughts and anxiety as well as fatigue. These are normal feelings caused by rapid changes in hormone levels. Factors such as lack of sleep, fatigue and feelings of isolation (from both work and social life) contribute to these feelings.
The lifestyle change and adjustment can also bring about many emotions for the other parent, which may be difficult to handle.
Signs of postpartum depression include:
- sleep disturbances (even when the baby is asleep)
- excessive worrying (inability to stop worrying even when the baby is fine)
- feelings of guilt
- a range of emotions (especially anger and sadness)
- loss of interests and joy in life
- inability to cope with daily life
Anxiety disorders can also develop after childbirth.
Postpartum depression and anxiety disorders can occur together.
If you experience symptoms of anxiety or depression, contact a mental health professional, midwife, family doctor or obstetrician.
Postpartum mood and anxiety disorders can be treated.
CONDITIONS FOR WHICH TO GO TO THE EMERGENCY DEPARTMENT
If you experience any of the following conditions within two months of giving birth, seek emergency care at the women’s clinic:
- severe headache, especially after the use of epidural analgesia in childbirth
- fever over 38 °C and chills
- uterine bleeding
- severe lower abdominal pain
- redness and swelling of the caesarean section wound
- foul-smelling or purulent discharge from the vagina
- redness and pain in the breasts
- breathing difficulties
- noticeable swelling of the limbs
POSTPARTUM CHECK-UP WITH A DOCTOR OR MIDWIFE
Two months after childbirth, attend a postpartum check-up where the healing of perineal stitches will be assessed and recommendations for breastfeeding and contraceptive methods will be provided. You can register for the appointment on weekdays by calling +372 666 1900 or via the health portal at terviseportaal.ee.
ITK773
Approved by the decision of the Care Quality Commission of Aktsiaselts Ida-Tallinna Keskhaigla on 11.12.2024 (protocol no. 17-24)
 Terviseportaal
Terviseportaal